
Autoimmune disorders comprise several diseases in which the immune system mistakenly attacks and destroys the body’s own healthy cells instead of destroying bacteria and viruses to keep the body healthy. Various factors are implicated in the pathogenesis of autoimmune disorders such as the environment, xenobiotics, food, stress, climate change, infections, genetic, and hormone disturbances. However, the exact mechanism for the development of autoimmune disorders is unknown. The impact of autoimmune disorders on societal, personal, and healthcare costs as well as on quality of life of affected patients is considerable, necessitating the development of suitable therapies for them. Autoimmune disorders have been shown to affect an estimated 4.5% of the population in 2021 with increasing rates between 3-9% per year. Although there are more than 80 different autoimmune disorders with varying symptomology and different effects on the body, some of the most common ones include type 1 diabetes mellitus (T1DM), rheumatoid arthritis, Grave’s disease, psoriasis, ankylosing spondylitis, multiple sclerosis, Crohn’s disease, ulcerative colitis, scleroderma, celiac disease, Sjogren’s syndrome, inflammatory bowel disease (IBD), systemic lupus erythematosus, and eczema.
The most common treatment options for autoimmune diseases include the following
Immunosuppressants
These decrease immune system activity and reduce inflammation and attack on healthy cells that helps in protecting organ function. Examples include low-dose chemotherapeutic agents (methotrexate, cyclosporin), corticosteroids, and biological agents such as monoclonal antibodies, tumour necrosis factor (TNF) inhibitors, Janus kinase (JAK) inhibitors, interleukin blockers (IL-1 and IL-6 blockers), T-cell inhibitors
Over-the-counter (OTC)
Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) to help relieve pain and inflammation. These include ibuprofen, meloxicam, and naproxen.
Plasmapheresis
This procedure involves a plasma exchange whereby plasma containing autoantibodies is removed and replaced with donated plasma or plasma substitute.
Immunoglobulin intravenous infusion
This consists of a pooled antibody used to modulate the immune system and reduce autoantibodies.
Lifestyle and dietary modifications
Regular exercise, sleep and stress management, balanced diet, and physical therapy can help manage symptoms and help in maintaining the overall well-being of patients with certain types of autoimmune diseases.
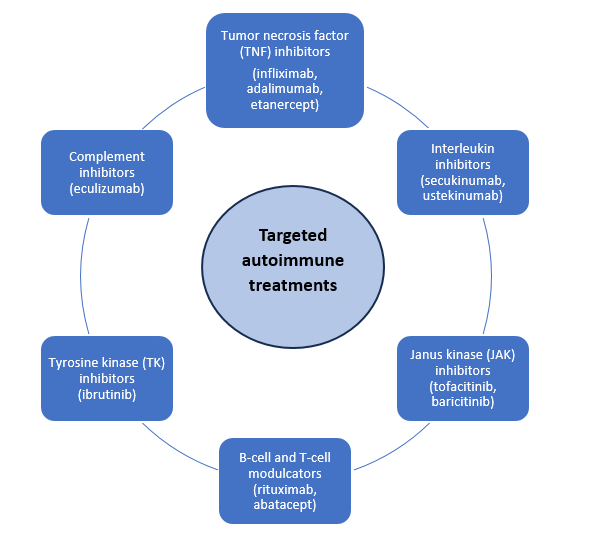
Figure. Targeted treatments for autoimmune disorders
Despite being an important component of autoimmune disorder management, most of the above-mentioned treatments are useful at managing the symptoms of these diseases. However, some drugs such as immunosuppressants are riddled with side effects such as increased susceptibility to infections, osteoporosis, weight gain, and gastrointestinal issues. In addition, long-term treatment can be expensive and offer only partial relief in some individuals while being ineffective as the disease progresses. Therefore, it is necessary to develop targeted and personalized treatments for autoimmune diseases which have minimal side effects by preventing damage to healthy cells. Recent and ongoing research efforts have focused on targeted therapies that block specific components of the immune process as depicted in the figure below.
Biological agents, selective chemical and small molecule, inhibitors and non-steroidal agents are becoming the focus of new treatment development for autoimmune disorders because of their better safety profile and improved responses in patients.
Some of the recently approved drugs for autoimmune disorders by the United States Food and Drug Administration (FDA) from 2020-2023 include:
1) Ravulizumab, a CS complement inhibitor for generalized myasthenia gravis
2) Rinvoq, a selective a reversible JAK inhibitor for Crohn’s disease and ulcerative colitis
3) Deucravacinitib, a selective TK inhibitor for plaque psoriasis and psoriasis
4) Tapinarof, a novel, non-steroidal, aryl hydrocarbon receptor modulating agent for plaque psoriasis
5) Efgartigimod, a neonatal Fc receptor blocker for generalized myasthenia gravis
6) Spesolimab, a IL-36 receptor antagonist for generalized pustular psoriasis flares
The table below enlists some drugs that are under clinical trials in USA (United States) for the treatment of some of the most common autoimmune disorders-namely, myasthenia gravis, rheumatoid arthritis, psoriasis, multiple sclerosis, T1DM, and Sjörgen’s syndrome.
| Drug treatment | Indication | Phase of clinical development |
| Rapamycin | Uveitis, systemic lupus erythematosus | 2 |
| Fenebrutinib | Multiple sclerosis | 3 |
| Evobrutinib | Relapsing multiple sclerosis | 3 |
| Tolebrutinib | Relapsing multiple sclerosis | 3 |
| Rozanolixizumab | Myasthenia gravis | BLA |
| Batoclimab | Myasthenia gravis | 3 |
| Sartralizumab | Myasthenia gravis | 3 |
| MuSK chimeric autoAb receptor T-cells (MuSK-CAART) | Myasthenia gravis | Preclinical |
| Haematopoietic stem cell | Myasthenia gravis | 1 |
| Peresolimab | Rheumatoid arthritis | 2a |
| IHL-675a | Rheumatoid arthritis | 2 |
| Otilimab | Rheumatoid arthritis | 3 |
| Olokizumab | Rheumatoid arthritis | 3 |
| Otelixizumab | T1DM | 3 |
| IMCY-0098 peptide | T1DM | 1b |
| Remibrutinib | Sjogren’s syndrome | 2 |
| Dazodalibep | Sjogren’s syndrome | 2 |
| Repegaldesleukin | Systemic lupus erythematosus | 2 |
| Lenabasum | Systemic lupus erythematosus and dermatomyositis | 3 |
| Etrasimod | Ulcerative colitis | NDA |
| Bimekizumab | Plaque psoriasis | BLA |
NDA: New Drug Application; BLA: Biologics License Application
Read More
Clinical Trial Regulations in the United States
References
2) Challenges, Progress, and Prospects of Developing Therapies to Treat Autoimmune Diseases (cell.com)
3) The Terrible Toll of 76 Autoimmune Diseases – Scientific American




