Endocrine disorders result from the improper functioning of endocrine glands that secrete and regulate hormones responsible for functioning of various organs. Imbalances in hormones or inability of the body to respond these hormones in a normal manner can result in several disorders. An estimated 5% of adults in the United States are affected by endocrine disorders as per 2022 prevalence estimated with diabetes being the most common. Endocrine disorders have a significant negative impact on public health from an epidemiological point of view and are associated with long-term disability, impaired quality-of-life, and mortality.
The most common endocrine disorders include the following
Hyperthyroidism and hypothyroidism
These are caused by overproduction and underproduction of thyroid hormones respectively leading to weight fluctuations and temperature intolerances.
Cushing’s syndrome
Caused by prolonged exposure or overproduction of cortisol hormone leading to weight gain, rounded face (“moon” face), and thinning of skin.
Growth hormone deficiency
Also known as dwarfism or pituitary dwarfism is caused by insufficient amounts of growth hormone in the body leading to short stature.
Polycystic ovary syndrome (PCOS)
Occurs in women of reproductive age caused by excess of androgen and causes menstrual irregularities, excess hair growth, and obesity.
Diabetes
Caused by failure of the pancreas to produce enough insulin or inability of the body to respond to insulin
The treatment protocol for endocrine disorders involves endocrine surgery to remove the diseased gland, medications to restore hormone levels and offer symptomatic relief, and lifestyle modifications.
Of the endocrine disorders, diabetes is the most common with increasing prevalence estimates globally. Childhood obesity, increased inactivity, access to processed foods, and ageing are some factors for the increase in worldwide estimates of diabetes and it is being touted as the greatest ‘epidemic’ in human history. Diabetes is associated with a higher risk of cardiovascular and renal complications such as heart attacks, strokes, and kidney failure making it necessary to diagnose the condition in a timely manner and manage it appropriately to avoid serious consequences. The management of type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) differs with insulin being used to manage T1DM and dietary control, exercise, medications, and insulin for T2DM.
Some of the recently approved drugs for diabetes by the United States Food and Drug Administration (FDA) from 2020-2023 include:
Terzepatide, a novel glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist for T2DM
Teplizumab, humanized IgG1 kappa CD3-directed monoclonal antibody that is used to delay progression of stage 2 T1DM to stage 3
Bexagliflozin, a sodium-glucose co-transporter 2 inhibitor to improve glycemic control in T2DM
Medtronic MiniMed 780G, an advanced hybrid-closed loop system for management of T1DM
Finerenone, a nonsteroidal, selective mineralocorticoid receptor antagonist for treatment of loss in kidney function or chronic kidney disease in T2DM
Semglee, insulin glargine (long-acting) for control high blood sugar in T1DM in children and T2DM in adults
Lantidra, allogenic pancreatic islet cellular therapy for T1DM patients
Despite, the various pharmacological and insulin management approaches in diabetes, some challenges remain in diabetes management. These include fluctuations in blood glucose levels using traditional insulin delivery systems, cumbersome insulin delivery methods, patient adherence to multiple medications, discomfort and inaccuracy associated with continuous glucose monitoring (CGM) systems, and lack of patient education and awareness as well as technological access.
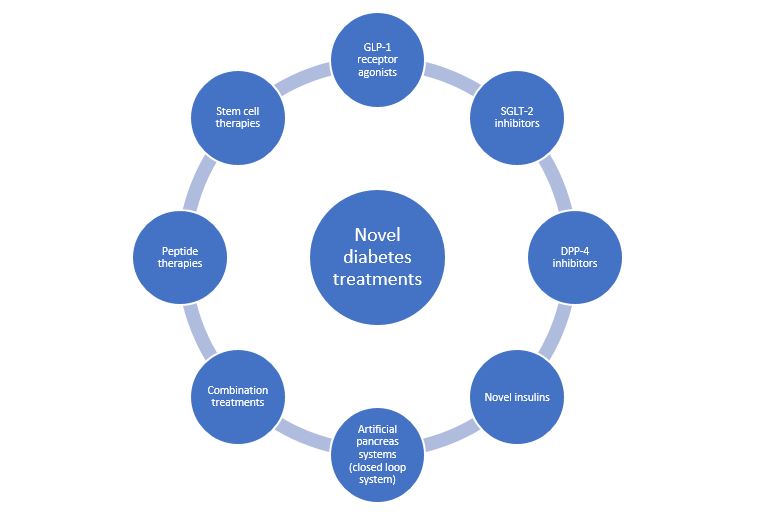
Therefore, novel treatments for diabetes have been developed with the aim of reducing side effects, avoiding blood glucose excursions to prevent hyperglycemia or hypoglycemia, improved cardiovascular and renal outcomes, longer-lasting effects avoiding administration multiple times a day, and innovative delivery methods that are non-invasive thus enhancing patient comfort and adherence.
Figure 1 depicts the novel treatments in the field of diabetology.
Glucagon-like peptide-1 (GLP) receptor agonists
These drugs mimic the action of the hormone glucagon-like peptide at the GLP-1 receptor in the pancreas and enhance insulin release in a glucose-dependent manner. They are indicated for the treatment of T2DM and help avoid hypoglycaemia. Some US FDA approved GLP-1 agonists include dulaglutide, exenatide, semaglutide, and liraglutide and are administered through the injectable route daily or weekly.
Sodium-glucose transport protein 2 (SGLT2) inhibitors
Drugs in this class reduce glucose reabsorption resulting in a decrease in blood glucose without affecting insulin levels. They are used in patients with T1DM and T2DM as add-on therapy with insulin. Cangliflozin, dapagliflozin, empagliflozin, and ertugliflozin are some FDA approved SGLT2 inhibitors.
Dipeptidyl peptidase 4 (DPP-4) inhibitors
These oral drugs act through increase of incretin hormones by blocking the enzyme DPP which in turn inhibits glucagon release and stimulates insulin secretion. Sitagliptin, saxagliptin, linagliptin are some FDA approved DPP-4 inhibitors
Novel insulins
Insulin therapy remains the mainstay for treatment of T1DM but traditional insulins suffer from challenges such as maintenance of safe glucose levels and time to action of insulins. Novel insulins are being developed to overcome these challenges and include ultra-rapid insulin which works faster and smart insulin that respond to blood glucose levels thus avoiding adverse glycaemic events.
Artificial pancreas system
This system consists of a continuous glucose monitor (CGM) and an insulin infusion pump and allows for real-time automatic monitoring of blood glucose levels and insulin delivery when needed in the form of a closed loop. Some of these systems (hybrid systems) often require the user to enter carbohydrate consumption at mealtime to calculate insulin delivery and are used by patients with T1DM. The FDA has recently approved the iLet Bionic Pancreas System for use in paediatric patients and has also approved the Medtronic MiniMed 670G system.
Combination treatments
These include drugs that provide a synergistic effect and are useful when any single drug is not able to provide adequate control or results in untoward effects such as hypoglycemia. Some combinations include GLP-1 agonists, SGLT-2 inhibitors, DPP-4 inhibitors with basal insulins, metformin, and bariatric surgery.
Peptide therapies
Glucagon-like peptide-1 receptor agonists (GLP-1RA) and
C-peptides can help manage insulin levels, inflammation, weight loss, and inhibition of enzymes that are involved in diabetes progression. They are generally available as injectable formulations because of their degradation in the gastrointestinal tract. Mounjaro, which is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like GLP-1 agonist was approved by the FDA in 2022 and is the first peptide drug of its class.
Stem cell therapies
This treatment involves the generation or restoration of the function of insulin-producing pancreatic beta cells. Research efforts are largely focused on mesenchymal stem cells (MSCs) for T1DM based on their potential to modulate hemoglobin A1c levels and C-peptide levels.
The table below enlists some drugs that are under clinical trials in the United States for the treatment of diabetes.
| Drug/treatment | Mechanism | Indication | Phase of clinical development |
| Enavogliflozin | Selective SGLT2 inhibitor | T2DM | 3 |
| Golimumab | Anti-TNF agent | T1DM | 2 |
| Dasiglucagon | Glucagon analogue | T1DM | 3 |
| ENT-001 | Recombinant protein | T1DM | 1 |
| CPP-1X-T (Eflornithine) | Decarboxylase inhibitor | T1DM | 2 |
| REMD-477 | Glucagon receptor antagonist | T1DM | 1 |
| AVT-001 | Dendritic cell therapy | T1DM | 1/2 |
| Cotadutide | Glucagon like peptide-1 and glucagon receptor agonist | T1DM | 2a |
| Ladarixin | IL-8 receptor inhibitor | T1DM | 2/3 |
| Mazdutide | GLP-1 and glucagon receptor activator | T2DM | 3 |
| Orforglipron | Nonpeptide GLP-1 receptor agonist | T2DM | 3 |
| VCTX-211 | Stem cell therapy | T1DM | 2 |
Read More
Ophthalmology disorders and current developments of novel treatments under clinical trials
References
- Artificial Pancreas – NIDDK (nih.gov)
- FDA Approves Novel, Dual-Targeted Treatment for Type 2 Diabetes | FDA
- Novel insulins – JDRF
- Biosimilars and Novel Insulins – PubMed (nih.gov)
- Novel and emerging therapeutic drug targets for management of type 2 Diabetes Mellitus – ScienceDirect
- An update on peptide-based therapies for type 2 diabetes and obesity – ScienceDirect