Data analytics, technology, and accessibility to the internet and healthcare has led to a paradigm shift in the way clinical trials have been conducted. Traditional clinical trials that have been used long since to generate data in support for approval of drugs, biological products, and medical devices, have historically used traditional methods for data collection, analysis, and storage or clinical data management (CDM) activities. Challenges to paper-based collection of data and data transcription are evident and limited by factors such as the experience and skill of professionals with data handling. Technological advancements have led to centralization of data management allowing data collection and storage from different sites to be performed in a secure and efficient manner. Electronic data capture (EDC) systems are widely used in present clinical trials that help streamline the process of collecting, storing, and securing data from multiple studies along with electronic case report forms (eCRF) and electronic clinical outcome assessment (eCOA), electronic patient-reported outcome (ePRO), electronic trial master file (eTMF), and e-consent.
These software systems are particularly useful for the decentralized clinical trial format that has gained popularity particularly after the COVID-19 pandemic. Nowadays, decentralized or hybrid trials in which some or all the trial activities are conducted remotely are widely used based on their several advantages such as improved patient recruitment and engagement, cost-effectiveness, real-time data collection, and more representative trial outcomes. Although advancements have been made in the design and conduct of trials, CDM activities are still catching up with these changes and need to evolve at the same pace to realize completely the benefits of these trial designs.
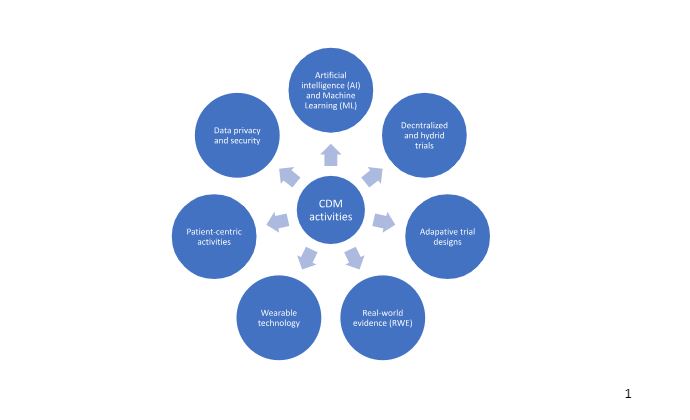
It is expected that the future if CDM will be driven by the following changes in trial design and conduct and data analysis as shown in the figure below:
Artificial intelligence (AI) and Machine learning (ML)
Processing vast amount of data from disparate sources to extract meaningful insights, trends, and patterns in relation to demographics, comorbidities, and adverse events requires ‘big’ data analytics and AI. CDM in the future would require employment of advanced data analytical techniques to deal with this vast amount of information. Natural language processing (NLP) algorithms are expected to be used to process large volumes of data and detect correlations in clinical data as well as extract insights from clinical notes written by physicians and healthcare professionals.
Decentralized and hybrid trials
CDM is likely to be shaped by trials that involve remote recruitment and monitoring of patients. Collection of health data from wearable devices such as mobile phones, smart watches, and telemedicine platforms requires a centralized system for collection and integration of data such as cloud-based systems.
Adaptive trial designs
These designs are unique as they involve mid-trial modifications or stoppage based ongoing information regarding the safety and efficacy of the product. Data collection, processing, and analysis should be flexible to allow documentation and feedback to the trial from these changes. Adaptive designs are commonly used in oncology and immunology trials which are complex and for ethical reasons.
Real-world evidence (RWE)
RWE studies are expected to be increasingly used in health-care decision making as they are representative of the real-world usage of a drug and safety concerns and provide monitoring of patients in real-time. Modification of data management services to accommodate RWE will include standardization of data from disparate sources and submission to regulatory authorities in conjunction with data from traditional clinical trials to make reliable decisions regarding product benefits.
Wearable technology
Increased accessibility and patient knowledge of health-tracking wearable devices involves data generation and sharing of a large volume of information that can be overwhelming to handle in the absence of suitable data analytics technology. Thus, management of data received from patients directly not only will need to be adequately handled and processed but also managed securely. Data privacy software, de-identification tools for data sets, and restricted accessibility to sensitive patient information will be the need of the hour in CDM practices.
Patient-centric activities
Clinical trials are moving from a central data management approach where investigators collect data and analyze it to a more patient-oriented approach where patients report their clinical outcomes and experiences allowing for a more complete understanding of product experience. It is important for CDM systems to be able to robust enough to securely access and interpret patient reports in an objective manner and develop validated PROs for use by patients.
Data privacy and security
The shift from traditional trials to use of remote monitoring, wearable sensors, telemedicine, and RWE studies that involve data sharing causes data security breach concerns which can compromise the reliability of trials and place patients at risk of losing sensitive information. Since the well-being and protection of human subjects is crucial for all trials, it is necessary for adequate data protection measures to be in place. Cybersecurity measures utilizing enhanced encryption technology, blockchain, and consent management systems will emerge important in CDM in the future.
Read More: The Impact of Real-World Evidence on Clinical Data Management
References
- Data management in clinical research: An overview – PMC (nih.gov)
- The Evolving Role of Decentralized Clinical Trials and Digital Health Technologies | FDA
- Real-world data: a brief review of the methods, applications, challenges and opportunities | BMC Medical Research Methodology | Full Text (biomedcentral.com)